Abstract
Chimeric antigen receptor (CAR) T-cell therapy targeting CD19 (CART19) has shown remarkable overall response rates in the treatment of hematological malignancies. However, durable response rates remain at approximately 40%. CART cell in vivo functions depend on their associated cell fate following infusion. T-cell exhaustion is an acquired and epigenetically regulated state of dysfunction that is associated with decreased proliferation and efficacy. While this phenomenon is widely considered a major limitation of CART cell therapy, mechanisms of CART cell exhaustion are poorly understood and vary depending on construct design and disease settings. Second generation CART19 cells with a CD28 costimulatory domain (CART19-28ζ) exhibit reduced persistence as compared to CART19 cells with a 4-1BB costimulatory domain. In this study, we aimed to interrogate the epigenetic landscape of exhaustion in CART19-28ζ cells. To ensure rigor, we employed the following three independent strategies: 1) RNA and ATAC sequencing on unstimulated vs. exhausted healthy donor CART19-28ζ cells by utilizing an in vitro model for exhaustion, 2) RNA and ATAC sequencing on pre-infusion axi-cel cell products from patients with B cell lymphoma treated in the pivotal Zuma-1 clinical trial that led to the FDA approval of axi-cel, comparing responders to non-responders, 3) a genome-wide CRISPR knockout screen in healthy donor CART19-28ζ cells.
To begin our studies, we developed a 14-day in vitro repeated stimulation assay with healthy donor CART19-28ζ cells to model antigen-driven exhaustion. After 7 days of repeated stimulation through the CAR with the CD19+ tumor cell line, JeKo-1, CART19-28ζ cells demonstrated phenotypic and functional hallmarks of exhaustion as compared to baseline CART19-28ζ cells, as characterized by: 1) upregulated inhibitory receptors (PD-1: p <0.0001, TIM-3: p <0.0001, and LAG-3: p = 0.02), 2) decreased proliferation (p <0.0001), 3) CD4 loss (p < 0.0001), and 4) a decrease in the percent of cells with positive intracellular staining for stimulatory and effector cytokines (IL-2: p <0.0001 and TNF-α: p <0.0001). RNA sequencing identified 449 significantly upregulated genes and 320 significantly downregulated genes in exhausted CART19-28ζ cells. ATAC sequencing identified 411 gene regions with increased accessibility and 445 gene regions with decreased accessibility.
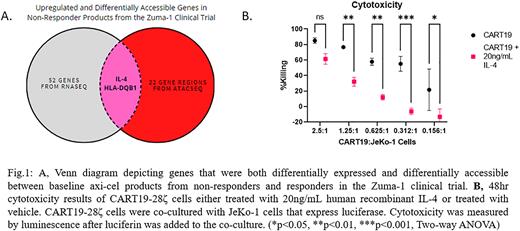
Overlap of RNA and ATAC results showed 105 genes that were both differentially expressed and differentially accessible. Ingenuity pathway analysis of these genes showed activation of the T-cell exhaustion pathway (p = 0.004, Z= 1.0), a potential role for the Th1 and Th2 activation pathway (p < 0.0001) and identified IL-4 as a significant upstream regulator of exhaustion (p < 0.0001). Next, we studied the transcriptional and epigenetic signature of baseline axi-cel products by comparing responders, patients who achieved a complete remission as best response, to non-responders, patients who achieved stable or progressive disease as best response. RNA sequencing showed 54 differentially expressed genes and ATAC sequencing showed 24 differentially accessible gene regions. Only two genes, IL-4 and HLA-DQB1, were upregulated in non-responders based on both RNA and ATAC sequencing data (Figure 1A). Then, by using our in vitro exhaustion model to conduct a genome-wide CRISPR knockout screen in CART19-28ζ cells from healthy donors, we saw enrichment of genes involved in the suppression of IL-4- mediated signaling as identified by gene ontology enrichment analysis (p = 0.0001).
Finally, to validate the functional impact of IL-4 on CART cells, we assessed effector functions of healthy donor CART19-28ζ cells following treatment with human recombinant IL-4. CART19-28ζ cells co-cultured with JeKo-1 in the presence of human recombinant IL-4 exhibited a reduction in antigen specific proliferation (p = 0.027), an increase in inhibitory receptor expression (TIM-3: p = 0.002 and LAG-3: p = 0.007), and a decrease in cytotoxicity as compared to vehicle treated cells (Figure 1B). IL-4 induced CART19-28ζ cell modulation was not due to a direct impact on tumor cells as identified by no change in tumor cytotoxicity or proliferation when JeKo-1 cells alone were treated with human recombinant IL-4. Together, this data suggests that the IL-4 axis may function as a key regulator of CART19 therapy failure associated with CART cell exhaustion.
Disclosures
Cox:Humanigen: Patents & Royalties. Sakemura:Humanigen: Patents & Royalties. Kim:Gilead Sciences Inc.: Current Employment. Mattie:Gilead Sciences Inc.: Current Employment. Scholler:Gilead Sciences Inc.: Current Employment. Filosto:Kite, a Gilead Company: Current Employment, Current equity holder in publicly-traded company; Tusk Therapeutics: Patents & Royalties. Kenderian:Mettaforge: Patents & Royalties; MustangBio: Patents & Royalties; Lentigen: Research Funding; Novartis: Consultancy, Patents & Royalties: CART cell therapy , Research Funding, Speakers Bureau; Morphosys: Research Funding; Juno/BMS: Consultancy, Research Funding, Speakers Bureau; Kite/Gilead: Consultancy, Research Funding, Speakers Bureau; Humanigen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties: CART cell therapy , Research Funding, Speakers Bureau; LEAH Labs: Current holder of stock options in a privately-held company, Research Funding; Tolero: Research Funding; Viracta/Sunesis: Research Funding; Life Engine: Current holder of stock options in a privately-held company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal